Health
Researchers Unveil 3D-Printed Heart Patch to Regenerate Tissue
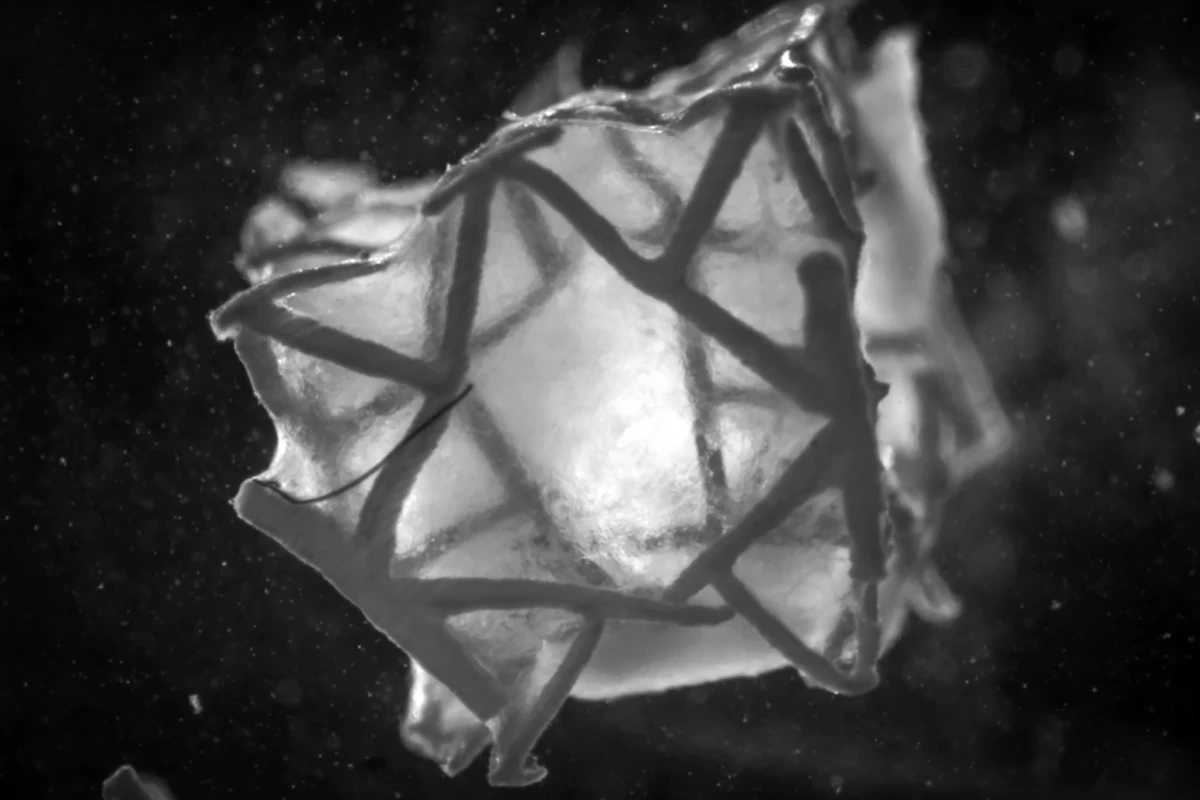
A team of researchers from ETH Zurich in Switzerland has developed a groundbreaking 3D-printed, biodegradable heart patch that not only seals holes in heart tissue but also promotes tissue regeneration. This innovative patch, called the RCPatch, presents a potential advancement over existing surgical materials used in cardiac procedures.
Heart disease remains the leading cause of death globally, with heart attacks significantly damaging heart cells and leading to scar tissue formation. In severe cases, ruptures in the heart wall may necessitate emergency surgical intervention. For years, scientists have created various implantable patches to address these challenges, but the new research promises to enhance the effectiveness of these solutions.
The study was led by bioengineering researcher Lewis Jones, who emphasized that traditional heart patches often fail to integrate with heart tissue, remaining as foreign objects within the body. “We wanted to solve this problem with our patch, which integrates into the existing heart tissue,” Jones stated.
Alongside Jones, corresponding author Professor Robert Katzschmann, PhD, expressed their ambition to design a patch that not only closes a defect but also contributes to complete repair.
The RCPatch is constructed from a biodegradable, biocompatible polyester metamaterial scaffold with adjustable stiffness to match the properties of surrounding heart tissue. The team utilized generative computer modeling to design hundreds of potential 3D lattice structures, ultimately selecting one that provided mechanical characteristics akin to the heart.
Infused within the scaffold is a fibrin-based hydrogel containing induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs), which are lab-grown heart muscle cells derived from adult cells. To enhance its functionality, a mesh infused with fibrin hydrogel was added, designed to minimize blood leakage while providing a surface suitable for surgical attachment.
“The scaffold is stable enough and can be filled with a hydrogel containing living cells,” Jones remarked. “The big advantage is that the scaffold is completely degraded after the cells have combined with the tissue. This means that no foreign body remains.”
The researchers cultured the RCPatch in the laboratory until the heart cells began contracting, achieving this milestone within approximately three days. They then evaluated the patch’s durability under conditions simulating heartbeats by subjecting it to repeated stretching and compression for thousands of cycles.
The final phase of the testing involved implanting the patch over an 8-mm (0.3-inch) hole in the left ventricle of a pig’s heart. Footage from the procedure demonstrated that bleeding from the ventricular hole ceased almost immediately upon application of the patch, with only minor bleeding persisting for about ten minutes. “We were able to show that the patch retains its structural integrity even under real blood pressure,” Katzschmann noted.
Despite the promising results, the study has limitations, primarily being an early-stage proof-of-concept tested in a single animal over a short time frame. Moreover, the researchers acknowledged that actual ruptures in ventricles may be larger and more irregular than the model used in their experiment. It remains uncertain how the patch degrades and integrates into the heart tissue over extended periods.
Nonetheless, with further research and validation, the RCPatch could offer a biodegradable, regenerative alternative to conventional animal-derived heart patches. Its development holds the potential to improve repair outcomes for heart ventricle injuries, significantly reducing the risk of long-term complications associated with heart attacks.
The findings of this study were published in the journal Advanced Materials in March 2024, marking a significant step forward in cardiac medical technology. As researchers continue to refine this innovative approach, the future of heart repair may be on the cusp of a transformation.
-

 Lifestyle4 months ago
Lifestyle4 months agoLibraries Challenge Rising E-Book Costs Amid Growing Demand
-

 Sports3 months ago
Sports3 months agoTyreek Hill Responds to Tua Tagovailoa’s Comments on Team Dynamics
-

 Sports3 months ago
Sports3 months agoLiverpool Secures Agreement to Sign Young Striker Will Wright
-

 Lifestyle3 months ago
Lifestyle3 months agoSave Your Split Tomatoes: Expert Tips for Gardeners
-

 Lifestyle3 months ago
Lifestyle3 months agoPrincess Beatrice’s Daughter Athena Joins Siblings at London Parade
-

 World3 months ago
World3 months agoWinter Storms Lash New South Wales with Snow, Flood Risks
-

 Science4 months ago
Science4 months agoTrump Administration Moves to Repeal Key Climate Regulation
-

 Science2 months ago
Science2 months agoSan Francisco Hosts Unique Contest to Identify “Performative Males”
-

 Business4 months ago
Business4 months agoSoFi Technologies Shares Slip 2% Following Insider Stock Sale
-

 Science4 months ago
Science4 months agoNew Tool Reveals Link Between Horse Coat Condition and Parasites
-

 Sports3 months ago
Sports3 months agoElon Musk Sculpture Travels From Utah to Yosemite National Park
-

 Science4 months ago
Science4 months agoNew Study Confirms Humans Transported Stonehenge Bluestones









